Every single person in this world want to have a better lifestyle with a good health care. Unpreventably, as we grow older, it is a huge challenge to maintain quality of healthcare because ourselves will expose to many health issues. Aging population, for example, are growing to certain level which we could not imagine. In 2017, as reported by United Nations (UN), approximately 962 million people aged 60 or above across the globe which cover 13 per cent of the global population. The aging population is mounting at a rate of 3 per cent per year. Due to these, techniques and procedures to replace, restore, or regenerate bone have become a major concern for clinical necessity subjected to orthopaedic, spinal, dental, cranial, and maxillofacial surgery.
Aging contributed a lot of diseases especially for orthopaedic reconstructions such as arthritis, tumours, and trauma. Every year, intensifying incidence of bone and joint disorder unavoidable and for most people these are nightmare to them and could end-up to miserable life for severe cases. Surely, these encourage of high demand driven on bone implant accompanied by the increase in number of orthopaedics reconstructions in order to bring back their normal lifestyle.
The usage of bone implant unavoidable for most patient with physical injury, especially fractured cases. They will experience first painful surgery as the surgeon installed a bone implant. After recovery and rehabilitation process, once again, the bone implant needs to be removed. Then the patient has to undergo the second surgery which will result to another pain or else the bone implant will stay in their body forever.
Similarly, in the degenerative cases such as osteoarthritis and osteoporosis, the damaged bone required to be removed and replace with the bone implant (known as bone graft or bone scaffold). The commercially available bone-graft in the market have different types such as autografts, allografts and xenografts. However, there are a few cases reported that deficits exist in current surgical practice which exhibited a vital concern of donor site morbidity (autografts), and limited supply and possibility of pathogen transmission and immune rejection (allografts and xenografts).

Researchers have been investigated and explored new potential for bone scaffold application for decades. The advancement of materials and fabrication techniques have directed researchers to develop the new generation of synthetic bone scaffold to eliminate susceptibility of the drawbacks accompanied by the previous established bone grafts. Bone scaffold were developed by a wide range of the biomaterials such as polymer, ceramic and metal. The metallic biomaterials are widely used and mostly preferred due to their high strength for bone structural supports. Commercially biomedical implant are stainless steels, titanium, tantalum and cobalt chromium-based alloys which could not be resolved in human body. It means that this type of bone scaffold will remain in body unless go through the second surgery for removal.
Yes, we accept that it helps to solve the injury problems but not for pain that patients endure again and again. Here is where researchers must look in different angle. Rather than, the bone scaffold remains and need to be removed, why not this bone scaffold fulfils their purposes as structural support while bone fully recovered, then it will disappear totally. Mission accomplished, right? This is the paradigm shift that researcher have gone through to make impossible become reality.
Thanks to the advancement in biomaterials engineering, the biodegradable materials is the paradigm shift. It has attracted researchers to investigate a lot in favour of obtaining the ideal bone scaffolds which could served as structural supports and encourage new bone formation. During the process of bone healing, the bone scaffold slowly degrades or resolves completely.
Engineers as well as orthopaedic surgeon acknowledged the advantages of metallic biomaterials rather than polymer and ceramic. Interestingly, this has expanded to biodegradable metal which exhibit the most promising properties and can be used temporarily during bone healing process. In order to be well integrated with host tissue, bone scaffold is required to have biocompatible characteristics with adequate porosity and mechanical properties, which are important for tissues regenerations. A porous bone scaffold with tailored mechanical properties as cancellous bone replacement to ensure good integration and serve as load bearing. Uniquely, cancellous bone has a complexity of features and geometry to allow the bone remodelling process to continuously happen.
With these inspirations, Medical Devices and Technology Centre (MEDiTEC) take the opportunity to make this porous bone scaffold a reality to the patients. Up to date, there is not yet commercially available porous biodegradable bone scaffold. There are a few challenges needs to be solved. Researcher in MEDiTEC, Dr. Amir Putra and his team, have develop a method to evaluate the degradation of porous biodegradable bone scaffold. They established a test rig known as dynamic degradation for bone scaffold purposes to characterize and analysed the behaviour of biodegradable porous scaffold under human physiological condition.
This technique simulates the biomechanical cancellous bone which adapts to the mechanical loading from the cyclic motion of physiological activities such as walking, running and jumping. Previously, researchers around the globe working on the degradation of bone scaffold were using the static immersion techniques mainly as a gold standard of assessing the proposed bone scaffold. However, the beauty of dynamic degradation integrates the most crucial factor for bone to sustain their conditions which are fluid movement and cyclic loading.
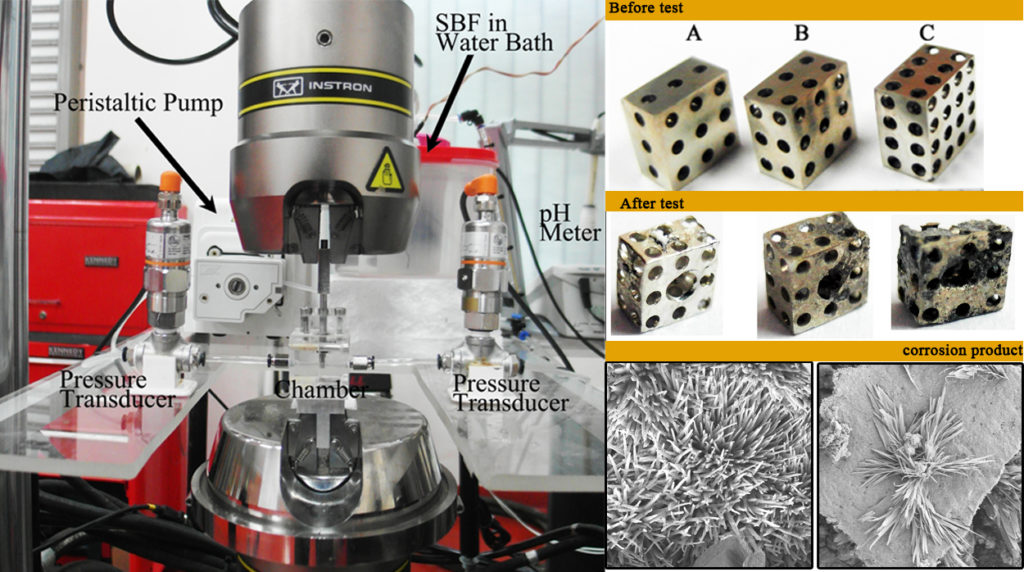
Currently, they have established the specify test rig for dynamic degradation purposes with variation of flow rates. This test rig also could perform with combination of loading which is simulating human physiological condition. Besides, they are rigorously working on the development of ideal bone scaffold architectural that tailored with cancellous bone properties. Not only by means of experimental work, they are enthusiastically working in computational approach as MEDiTEC has a well-established high-performance computational simulation lab.
Way forward, they are aiming to prove their developed product could benefit to the people. Patients will no longer have to experience second surgery through this product. This is the challenge that they take and paradigm shift that they endured to make dreams become reality.